Why Home-Based Sleep Testing Matters
Obstructive sleep apnoea (OSA) is a sleep-related breathing disorder in which repeated episodes of upper airway collapse lead to disrupted breathing, fragmented sleep, and intermittent drops in oxygen levels. While OSA is commonly discussed in adults, it also affects children and adolescents — and the way it presents, is diagnosed and managed differs in important ways.
Many families are understandably hesitant about traditional sleep studies in unfamiliar hospital environments. This is where home-based sleep testing — particularly an overnight oximetry or level two home sleep study — can play a crucial role, allowing children to sleep in their own beds and provide clinicians meaningful information about their breathing during sleep.
Overnight oximetry - probe placed on the big toe of a child
What Is OSA in Children and Adolescents?
In children and adolescents, OSA is characterised by repeated partial or complete blockage of the upper airway during sleep. These obstructions interrupt normal sleep architecture and can lead to oxygen desaturation, fragmented sleep and a range of daytime symptoms.
Unlike adults, where obesity and aging tissues are the dominant factors, OSA in young people often has different underlying causes.
Common Features in Children and Adolescents
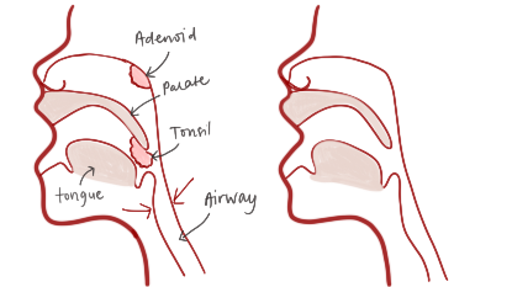
Upper airway anatomy in children
Enlarged tonsils and adenoids: These are among the most frequent contributors to airway obstruction in young children.
Craniofacial differences: Dental and jaw development can play a role.
Allergic rhinitis and nasal obstruction: Blocked nasal passages contribute to increased airway resistance.
Obesity: Becoming an increasingly recognised factor in adolescents, particularly in teenage years.
Neuromuscular or genetic conditions: In some children, other medical diagnoses increase the risk of OSA.
How Is OSA Different in Children Compared to Adults?
Though the basic mechanism of upper airway obstruction is shared between paediatric and adult OSA, there are key differences in symptoms, consequences and diagnosis.
Differences in Symptoms
Adults often report:
Loud snoring
Witnessed apnoeas (pauses in breathing)
Daytime sleepiness
Morning headaches
Children and adolescents may present differently:
Mouth breathing or restless sleep
Frequent night wakings
Bed-wetting
Irritability or behavioural issues
Difficulty concentrating or learning challenges
Poor growth or weight issues
In children, behavioural changes and daytime hyperactivity can be more noticeable than classic “sleepiness,” particularly in younger school-aged children.
Differences in Daytime Impact
OSA in young people can affect:
Cognitive function
School performance
Behaviour and attention
Growth and overall health
Because children are still developing physically and neurologically, untreated OSA can have greater long-term consequences than in adults.
Why Testing Is Important — and Why Home Matters
Diagnosing OSA requires monitoring breathing during sleep. The gold standard is in-lab or level one polysomnography, which is comprehensive but typically performed in a sleep laboratory in a hospital— a novel environment for a child that often disrupts normal sleep.
For many children, sleeping in a hospital environment is uncomfortable due to:
New surroundings
Strange lights and noises
Separation from family routines
This can alter sleep patterns during the test.
The Case for Home-Based Sleep Testing
Comfort and Familiarity
Children sleep in their own beds, surrounded by familiar sights, routines and security, which supports more natural sleep patterns.
2. Better Reflects Typical Sleep
Because a child’s sleep is less disrupted by unfamiliar environments, home tests may give clinicians a more accurate picture of sleep breathing.
3. Valuable Clinical Data
4. Less Stress for Families
For parents and carers, home testing:
Removes the anxiety of overnight hospital stays
Reduces logistical burden
Improves participation and cooperation
Helps keep bedtime routines intact
How Home Sleep Testing Works
Home sleep testing for children typically involves:
Placing a small, comfortable sensor on a finger or toe
Wearing a lightweight device overnight
Parents following simple setup instructions
Returning the device for clinical review the next day
Less intrusive than a full lab study, this type of test collects key physiological data while the child sleeps naturally at home.
Supporting Better Sleep in Children With Suspected OSA
Alongside testing, families can improve sleep quality through good sleep hygiene:
Maintain consistent bedtime and wake-up routines
Create a calm, quiet sleep environment
Reduce exposure to screens before bed
Address nasal obstruction and allergy symptoms proactively
These habits support children’s overall sleep health and optimise the conditions for restful sleep.
When to Seek Professional Evaluation
Parents and carers should consider a sleep assessment if a child experiences:
Loud snoring most nights
Pauses in breathing during sleep
Restless sleep or frequent night waking
Daytime behavioural changes, poor concentration or learning difficulties
Unexplained daytime fatigue or irritability
At Prana Paediatric Sleep Service, we help families navigate the evaluation and diagnosis of sleep-related breathing disorders. Home-based sleep testing is often an easy first step before considering airway surgery, that provides valuable insight while reducing stress for families.